Oral contraceptives are chemicals taken by mouth to inhibit normal fertility. All act on the hormonal system. Female oral contraceptives have been on the market since the early 1960s, and enjoy great popularity. They are used by millions of women around the world, though the acceptance varies by region: approximately one-third of sexually active women in the United Kingdom use them, but they are less widely used in countries such as Japan. Male oral contraceptives remain a subject of research and development, and are not widely available to the public.
Principles
Female oral contraceptives, colloquially known as the Pill, are the most common form of pharmaceutical contraception. They are used to prevent pregnancy. The pill is also used to control symptoms of polycystic ovary syndrome (PCOS) and endometriosis. Many doctors prescribe the Pill to women who complain of dysfunctional uterine bleeding.
Female oral contraceptives consist of a pill that women take daily and that contains doses of synthetic hormones (always a progestin and most often also an estrogen). In some types of pill the doses of hormones are adjusted to be in synchrony with the menstrual cycle (two- or three-phase pills), while others keep a constant level of the hormones.
Use
The Pill must be ingested daily, within 12 hours of the same time each day (for progesterone/estrogen pills – as opposed to within 3 hours for Progesterone only pills). Most brands are packaged with 21 days of active (hormone-containing) pills followed by either 7 days of placebo pills, or instructions to not take pills for seven days. A woman on the pill will have a withdrawal bleed, or period, sometime during the placebo week.
Mechanism of action
Several different types of ‘the Pill’ exist. Generally, they all have different synthetic estrogens and progestins, chemical analogues of the natural hormones, estradiol (an estrogen) and progesterone (a progestagen). Most common brands use 20 to 40 micrograms of ethinyl estradiol as the estrogen component and either a fixed or varying (the bi- and triphasic pills) amount of either levonorgestrel or norethindrone as the progestagen component.
Please see Progesterone only pills which, lacking any estrogen, have generally less side-effects and complications than combined pills.
The combined Pill prevents pregnancy primarily by preventing ovulation. It also has the side-effect of thickening the mucous over the cervix, which can prevent or slow sperm entry into the uterus. The Pill also thins the endometrium (the lining of the uterus).
There are physicians who point to this thinning of the endometrium as evidence that The Pill is an abortifacient. This claim is based on experiences with in vitro fertilisation which demonstrated that thinner uterine linings correlated with increased difficulty in getting the test-tube-fertilized eggs to implant. However, many more physicians (including some pro-life physicians) are unconvinced that this truly does decrease the likelihood that a fertilized egg will implant itself in the uterine lining. The reason for this is that the thinner uterine linings were observed only when ovulation has not occurred. When ovulation occurs, the corpus luteum releases extremely large amounts of hormones —approximately ten to twenty times as much estrogen and progesterone as seen in a non-ovulatory pill cycle.
In women who do not take The Pill, the uterine lining is usually unreceptive to implantation prior to ovulation. The purpose of the hormones released by the corpus luteum is to cause the endomitrium to thicken and become receptive to implantation (which occurs between six and twelve days after ovulation if the ovum is fertilized). Thus, simple observations that the uterine lining is too thin to support implantation during a cycle where no ovulation has occurred is insufficient to support the claim that there is a reduced likelihood of implantation in ovulatory Pill cycles. Currently, no research has been conducted on the behavior of the endometrium in ovulatory Pill cycles. The medical consensus is that pregnancy starts with implantation, not fertilization, so even an anti-implantation effect would not make the pill an abortifacient.
Effectiveness
The Pearl Index is often used to compare the effectiveness of various methods of contraception. It is expressed as the “number of pregnancies in 100 normally fertile women over the period of one year”. Each method of birth control has two Pearl index numbers:
- method effectiveness: is the Pearl index number for use under perfect conditions. The method effectiveness Pearl index for the Pill has been measured as low as 0.3 and as high as 1.25, which means that under ideal conditions, anywhere from 0.3 to 1.25 out of 100 users will become pregnant during one year of perfect use (Pearl index = 0.3 to 1.25).
- user effectiveness or typical effectiveness: is the Pearl index number for use that is not consistent or always correct. The user effectiveness measured by the Pearl index for the Pill has been measured as low as 2.15 and as high as 8.0, which means that anywhere from 2.15 to 8.0 out of 100 women will become pregnant during the first year of typical use (Pearl index = 2.15 to 8.0).
Many women occasionally forget to take the Pill daily, impairing its effectiveness. Correct use of the pill usually implies taking it every day at the same hour for 21 days, followed by a pause of seven days.
Use of other medications can prevent the Pill from working, due to interactions with the metabolism of the hormonal constituents. Diarrhea will also stop the Pill from working, because the hormones are not properly absorbed by the bowels.
While the Pill is usually effective, its wide availability has not prevented all unplanned pregnancies.
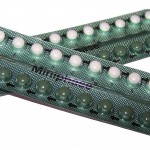
Packaging
The Pill usually comes in two different packet sizes, and each packet usually has days marked off for a cycle lasting of 28 days. For the 21-pill packet, a woman takes a pill each day for 21 days, and waits for an additional seven days before starting the next packet. For the 28-pill packet, the woman similarly takes a pill each day. However, instead of only taking pills for 21 days of the month, she also takes the remaining seven placebo or sugar pills included in the packet, and once she finishes the last placebo pill, she can immediately start the next packet on the following day.
The purpose of the placebo pills is to ensure that the woman, out of habit, can take a pill on every day of her menstrual cycle, so that she does not have to calculate when exactly is the next date that she should start her next packet of pills. If the pill formulation is monophasic, it is possible for a woman to skip menstruation and still remain protected against conception by skipping the placebo pills and going straight to the next packet.
Attempting this with bi- or tri-phasic pill formulations carries an increased risk of breakthrough bleeding and may be undesirable. It will not, however, increase a woman’s risk of becoming pregnant. The presence of placebo pills is thought to be comforting for the woman, as menstruation is a physical confirmation that she is still not pregnant. Breakthrough bleeding also becomes a more common side effect as a woman attempts to go longer periods of time between menstrual periods.
Drug interactions
Some drugs reduce the effect of the Pill and can cause breakthrough bleeding, or pregnancy (together with unprotected sex, of course). These include antibiotics, barbiturates, phenytoin and carbamazepine. The traditional medicinal herb St John’s Wort has also been implicated.
Side-effects
When starting to take the Pill some women report slight weight gain, although most studies show that the incidences of this is about 50% and as many women experience slight weight loss. Some women also notice changes in the intensity of sexual desire, vaginal discharge and menstrual flow.
Some other common side effects are: breakthrough bleeding, nausea, headaches, depression, vaginitis, urinary tract infection, changes in the breasts, changes in blood pressure, skin problems, skin improvements, and gum inflammation. The insert included with each pill packet usually has a more extensive list of recognized side effects.
Formulations
See oral contraceptive formulations
Effects on sexuality
The effect of the Pill on a woman’s sexuality are difficult to judge; depending on the individual and the particular formula, the Pill may enhance or disrupt a woman’s (or couple’s) sex life. Neither the woman who uses the Pill nor her partner need take any special action before or during intercourse, which makes birth control “invisible” and sex spontaneous and more natural. When combined with the Pill’s high degree of effectiveness, this may enable the couple, and especially the woman, to relax more easily during sex. Masters and Johnson, among others, reported more than one woman who experienced her first orgasm during intercourse shortly after going on the Pill.
On the other hand, the Pill’s various side effects may prove disruptive on a physiological or even a psychological level. The hormonal disruption caused by the Pill may result in mood swings, lower libido, excessive or insufficient vaginal lubrication during intercourse, and possibly an injured self-image due to weight gain. Some women who use the Pill despite the teachings of their religious traditions may feel conscious or unconscious guilt; others may not fully trust an “invisible” method of birth control. This wide range of variables makes prediction of the Pill’s effect on sexuality difficult, but the fact that the Pill can and does have an impact in this area, for good or for ill, is well-documented.
Cautions and contraindications
Oral contraceptives may influence coagulation, subtlely increasing the risk of deep venous thrombosis (DVT) and pulmonary embolism, stroke and myocardial infarction (heart attack). However, estrogen contraceptives are usually only contraindicated in women with pre-existing cardiovascular disease, in women who have a familial tendency to form blood clots (such as familial factor V Leiden), women with severe obesity and/or hypercholesterolaemia (high cholesterol level) and most notably in smokers.
Estrogen based pills have also been linked to an increased risk of breast cancer, although newer Pill types may not influence breast cancer risk. In rare cases, high estrogen Pills may trigger benign intracranial hypertension.
The chance of developing most of the above problems increases with age – especially when certain other health problems are present. The risks are even greater for women who are age thirty five or older, smoke more than fifteen cigarettes a day, or have conditions associated with heart attack, such as diabetes, high blood pressure, or high levels of cholesterol, and certain inherited conditions that increase the risk of blood clotting. Women using the Pill who undergo major surgery seem to have a greater chance of having blood clots.
Non-Contraceptive Uses
Aside from being a contraceptive, and controlling the symptoms of some hormonal disorders, many women use the Pill so their periods will be predictable (although the Pill does not treat many underlying causes of irregular cycles). There may also be incidental benefits to the Pill. There is some evidence that use of the pill might reduce the incidence of ovarian cancer and endometrial cancer. As there is also evidence that use of the pill may increase the risk of developing breast cancer or deep-vein thrombosis, individuals must do their own cost-benefit analyses.
The Pill is commonly used as Hormone Replacement Therapy by trans women. The oestrogen in the Pill is effective at blocking the effects of testosterone, and thus preventing further masculinisation, as well as promoting feminisation. Trans women typically use a far higher dose of the Pill than cis women in order to achieve feminisation, with 4 pills taken per day being commonplace.
Due to the possible side-effects of taking high doses of the Pill, such as liver or kidney damage, it is recommended that trans women consult their doctors for regular blood tests. Not all birth control or hormone pills work in exactly the same way so if one Pill is showing evidence of doing damage, switching to another form of birth control or hormone tablet can remedy the problem.
References
- Hormone Contraceptives: Controversies and Clarifications, by the American Association of Pro-Life Obstetricians and Gynecologists
- Pearl R., Factors in human fertility and their statistical evaluation. Lancet 1933;2:607-611.
- Data based on article: Audet MC, Moreau M, Koltun WD, Waldbaum AS, Shangold G, Fisher AC, Creasy GW. Evaluation of contraceptive efficacy and cycle control of a transdermal contraceptive patch vs an oral contraceptive: a randomized controlled trial. JAMA. 2001;285(18):2347-2354.
- Alan Guttmacher Institute, Facts in Brief, First Year Contraceptive Failure Rates
- Reduction in ovarian & endometrial cancer study.
- Hormonal contraceptive use in Japan, 2004 news article.
- Abortion Surveillance, CDC.
- Evolution and Revolution: The Past, Present, and Future of Contraception, Baylor College of Medicine, Houston, Texas.

Latest comments